2025 PMHNP Career Outlook: High Need, High Demand, Rising Salaries
- Oct. 14, 2024
Share:
The psychiatric-mental health specialty is the fastest-growing choice among nurse practitioner students, and the interest couldn’t come at a better time. The National Institute of Mental Health estimates that more than 1 in 5 U.S. adults is affected by a mental illness. Yet the supply of professionals trained to diagnose and treat mental health conditions cannot meet the demand.
The Health Resources and Services Administration (HRSA) reports that 123 million U.S. residents live in areas with a shortage of mental health professionals and estimates that 6,203 additional mental healthcare providers are needed. Psychiatric-mental health nurse practitioners (PMHNPs) can help fill this gap, and academic programs are ramping up to prepare NPs in this specialty.
Academic programs are hustling to meet the growing demand for PMHNPs
Over the past decade, universities have added nearly 100 tracks to prepare NPs to enter practice as a specialist in psychiatric-mental health. More than 13,000 new PMHNPs have graduated since 2012, the American Association of Colleges of Nursing (AACN) reports.
AACN’s 2023-2024 Enrollment and Graduation Report shows that during this academic year, 374 PMHNP programs are awarding MSN, MSN-to-DNP, and BS-to-DNP degrees. Verdi and Ainslee (2024) report that 27 are dual-track programs — four of which prepare students to sit for both family nurse practitioner and PMHNP certification. In their article, Verdi and Ainslee state the case for expanded development and utilization of dually certified FNP-PMHNPs who can provide holistic care that serves medical and mental health needs at the same visit.
Although the number of academic programs adding a PMHNP degree track is increasing, many more are needed, said Abby McNeil, DNP, FNP-BC, PMHNP-BC, one of the instructors for the PMHNP Review Course & Clinical Update developed by APEA.
“The psychiatric provider shortage is having a direct impact on our communities,” she said. “We need to provide a pipeline of educated PMHNPs to improve access to mental health care in underserved areas. But one of the difficulties in starting these programs is the lack of qualified PMHNP faculty to teach in the programs. The demand for programs and faculty will continue to grow."
PMHNPs are in high demand now and for the foreseeable future
The Bureau of Labor Statistics projects that employment opportunities for all mental health professionals will grow 3% faster than the average for all occupations. The analysis does not specify nurse practitioner job openings but reports a 7% increase in demand for psychiatrists. PMHNPs are likely reflected in that population and their scope of practice encompasses the diagnosis, treatment and pharmacologic management of patients with mental health conditions. (Nurse practitioners have prescriptive authority in all states and can manage psychopharmacologic regimens.)
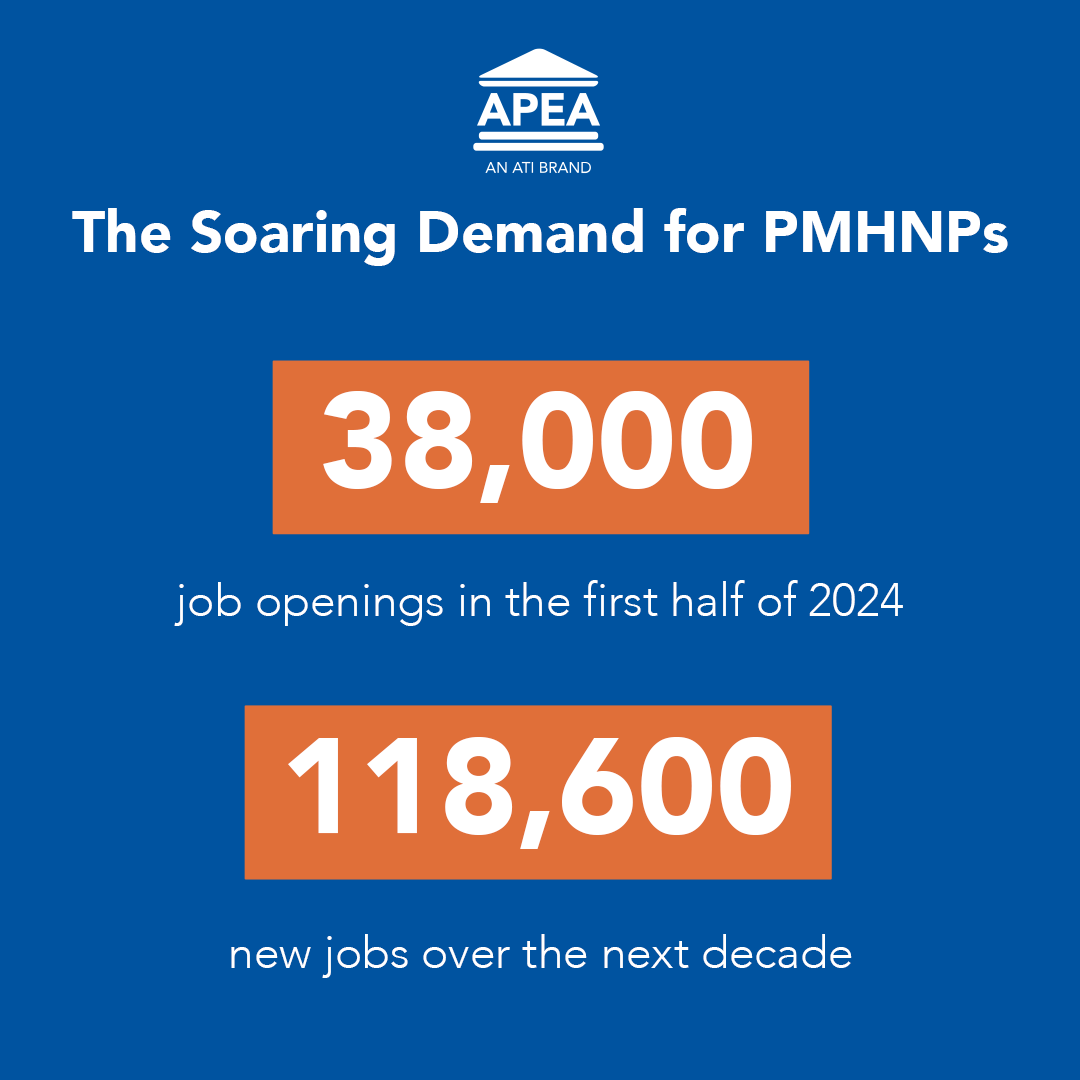
Other strong indicators of demand are abundant on job sites. For example, the Zippia career and jobs website identified more than 38,599 job openings for PMHNPs in the first half of 2024 and projects 118,600 new jobs for PMHNPs over the next decade.
The general willingness of nurse practitioners to work in underserved areas and to see patients insured by Medicare and Medicaid is also boosting the appeal of hiring PHMHNPs. An analysis published in Health Affairs in 2022 determined that the number of NPs treating Medicare beneficiaries for psychiatric and mental health conditions grew 162% between 2011 and 2019, compared with a 6% decrease in the number of psychiatrists treating Medicare patients.
In 2019, NPs provided between 34% and 51% of mental health office visits for Medicare beneficiaries in urban and rural areas where NPs have full practice authority. “PMHNPs are a rapidly growing workforce that may be instrumental in improving mental healthcare access,” the authors concluded.
Also contributing to an understanding of the career outlook for PMHNPs is a national survey by The American Psychiatric Nurses Association (APNA). The APNA 2022 Psychiatric-Mental Health Nursing Workforce Report is the first study of the psychiatric-mental health nursing workforce. This survey of more than 5,000 NPs and clinical nurse specialists focused on mental health found that:
- the average APRN in this specialty is 54 years old
- 27% plan to retire within the next 6 years
- 70% practice in outpatient settings including mental health clinics, federally qualified healthcare centers, and community health centers
- almost half reported treating patients insured by Medicare or Medicaid.
In the report, the APNA emphasized that providing services to the Medicare and Medicaid populations is critical because a significant percentage of patients with serious mental illnesses are insured by these programs and “psychiatrists have low acceptance rates of individuals on these plans.”
Noting that patients with serious mental illness require more complex management, the APNA cited evidence that APRNs who specialize in psychiatric-mental health “are well suited to provide care and address the significant unmet mental health care needs of this population.”
Returning to the editorial by Verdi and Ainslie (2024), dual training and certification in primary care and psychiatric-mental health could more fully meet the need for holistic care experienced by patients with complex needs and who are insured by federal and state programs.
"As medical and mental health diagnoses converge, dual-certified FNP and PMHNPs are uniquely situated to support these complex patients in a timely and holistic manner," the authors wrote.
Widespread need for PMHNPs is producing higher-than-average salaries
Meeting the growing demand for PMHNPs is a challenge that will continue. The Health Resources and Services Administration (HRSA) projects that the supply of PMHNPs will increase 17% between 2016 and 2030 but still not meet the demand for services.
Given the nationwide need for mental healthcare providers, PMHNPs earn salaries that are higher than the average salaries for all other NP specialties, several surveys show.
In its 2024 NP Salary Report, the healthcare staffing agency CompHealth reported that the PMHNPs it polled earned an average of $134,000 in 2022. Adult-gerontology acute care NPs came in a close second at $132,000. Primary care roles commanded the lowest salaries: Adult-gerontology primary care NPs earned an average of $129,000, and family nurse practitioners earned an average of $124,000.
Similarly, a 2023 survey of more than 1,000 NPs conducted by the advanced practice-focused publication Clinical Advisor found that PMHNPs earned $137,167 compared to $120,462 for FNPs and $119,877 for AGPCPs.
In a departure from these findings, the job website Indeed reported in September 2024 that the national average salary for PMHNPs was $105,403. However, several listings displayed prominently on the site listed much higher salaries: $232,909 in Chattanooga, Tenn., $213,395 in Baltimore, $213,395 in Portland, Ore., $201,064 in Seattle, and $200,650 in Waterbury, Conn. Over on the Zip Recruiter website on the same day, positions advertised PMHNP salaries of $154,381 in New York City and $165,000 in Washington, D.C.
How can you become a psychiatric-mental health nurse practitioner?
If you are motivated to care for patients with mental illness and reassured by the high projected demand and salary for PMHNPs, how do you get started on this path? Your journey begins with selecting the right academic program.
For nurses and nurse practitioners interested in specializing in psychiatric-mental healthcare, the first step is to research which academic programs have earned accreditation to award a PMHNP degree. Nursing programs earn accreditation from one of two organizations, the Commission on Collegiate Nursing Education (CCNE) or the Accreditation Commission for Education in Nursing (ACEN). Visit these websites to identify accredited PMHNP programs.
In addition to confirming national accreditation, determine whether the program curriculum aligns with the Consensus Model for APRN Regulation: Licensure, Accreditation, Certification and Education (LACE). This ensures that the education you will receive meets established standards for national certification and clinical practice by nurse practitioners.
When you’re selecting your academic program, also ask about the institution’s:
- pass rates on the PMHNP exams
- assistance with clinical placements (will you have to find your own, or does the program have established relationships with clinical sites?)
- tuition and fees.
Throughout your academic program, faculty recommend using study questions to build and reinforce knowledge and help determine mastery of course content. APEA has developed question banks to support students during the core courses of a PMHNP program (pathophysiology, pharmacology and physical assessment) and during the population-focused coursework (the psychiatric-mental health specialty content).
How can you earn national board certification as a PMHNP?
After completing an accredited PMHNP academic program, graduates move to the important step of earning national board certification. Two certifying bodies offer exams for the PMHNP specialty: the American Nurses Credentialing Center (ANCC) and the American Association of Nurse Practitioners Certification Board (AANPCB). Most employers require board certification because payers (insurance companies, Medicare, Medicaid) require it for reimbursement.
To sit for either PMHNP exam, candidates must:
- have a current active professional nursing license
- have earned a master's degree, postgraduate certificate, or doctoral degree from an accredited PMHNP program
- have completed a minimum of 500 faculty-supervised clinical hours in the PMHNP role.
See this article on the NP Insider Blog for details on the AANPCB exam for PMHNPs, which was introduced in 2024. For details on the ANCC exam for PMHNPs, visit this link.
To ensure you are prepared to take the ANCC or the AANPCB certification exam for PMHNPs, experts advise candidates to take a review course that reinforces key concepts from your PMHNP education and coaches you in how to be successful on the test. Select an up-to-date course that is based on current evidence-based clinical guidelines and the current certification exam.
“For PMHNP students to be successful in passing the certification exam, they must have a study plan that includes a PMHNP review course,” McNeil said. “An evidenced-based course such as the one developed by APEA provides a comprehensive review that reflects the content of the current PMHNP exams and provides valuable test-taking strategies. This sets students up for success.”
The PMHNP Review Course & Clinical Update released by APEA in September 2024 is the most up-to-date course available to prepare for both PMHNP exams.
APEA’s faculty of psychiatric-mental health specialists developed this on-demand course to prepare students for success on the PMHNP certification exams. The content reflects the blueprints (test design) for the PMHNP exams from ANCC and AANP but goes beyond this to provide the information and practical strategies students need to pass either PMHNP certification exam.
The APEA PMHNP Review Course is available in video and audio formats. It includes:
- 21 lectures delivered over 17 hours (17 contact hours; 12 pharmacology)
- a printable color Course Manual that serves as a study guide for your exam and a resource for clinical practice
- 3 views of every lecture within 6 months of purchase (video version) or 1 year of unlimited listening (audio version)
- rewind and fast-forward abilities to ensure understanding.
The course faculty are well-known for their mental health expertise and their engaging teaching styles that help students recall and retain key information for the exams. Shantell Jackson-Burns, DNP, ARNP, PMHNP-BC, Christy Cotner, DNP, MSN, PMHNP, FNP, and Abby McNeil, DNP, FNP-BC, PMHNP-BC.
Feedback from students who have completed the PMHNP Review Course from APEA show that the faculty, lectures and Course Manual helped solidify their understanding of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) criteria for diagnosing the most common psychiatric disorders. Importantly, students have stated that the faculty’s teaching methods helped them better understand the pharmacologic therapies and behavioral strategies necessary to manage the symptoms of mental illness.
"We developed this review course for PMHNP candidates using strategies that help ensure they will be successful on the certification exam and enter practice as competent and confident providers," Dr. McNeil said. "APEA's teaching methods have been proven effective over and over again, and our PMHNP faculty looks forward to hearing from the many new graduates who use this course to help prepare for their exam and for practice."
References
Cai A, et al. (2022). Trends In mental health care delivery by psychiatrists and nurse practitioners in medicare, 2011-19. Health Affairs. (2022), 41(9):1222-1230. doi: 10.1377/hlthaff.2022.00289
Health Resources and Service Administration Health Workforce. (n.d.). Behavioral health workforce projections, 2016-2030: Psychiatric nurse practitioners, psychiatric physician assistants. https://bhw.hrsa.gov/sites/default/files/bureau-health-workforce/data-research/physician-assistants-2018.pdf
Verdi, M, Ainslie, M. (2024). A call to action: Leveraging dual-certified APRNs to optimize holistic patient care. Journal of the American Association of Nurse Practitioners, 36 (10), 535-538. DOI: 10.1097/JXX.0000000000001064